State Health Officer Dr. Thomas Dobbs sees improvement in the fight against COVID-19 following the governor’s two-week mask mandate across Mississippi. But a return to in-person schooling presents grave danger. Photo courtesy Thomas Dobbs
State Health Officer Dr. Thomas Dobbs has overseen the Mississippi State Department of Health’s response to the coronavirus pandemic for half a year now. For the first time since the reopening of the state in late April, Dobbs sees the first signs of downward trends in key metrics—new cases and new hospital admissions. This is evidence that the state’s mask mandates and health messaging are having the intended effect, he says.
But Dobbs is also looking ahead to the imminent reopening of Mississippi’s schools and the threat it poses, a decision he cautioned the governor against to no avail. Other medical experts joined Dobbs in calling for the school delay, including the University of Mississippi Medical Center’s LouAnn Woodward and medical associations across the state.
Mississippi’s top health expert spoke with the Jackson Free Press on Aug. 12 about the state’s response.
Right now, our daily COVID-19 numbers look more like the beginning of July than the end of it. Is this a trend? What does it tell us?
I think we've pretty clearly seen some moderation in the case reports. I think it's real, and I'm certainly very happy to see it. It’s nothing to celebrate: It's still way too high. But I think it is a powerful indicator that if we can do some of those simple things ... maybe the masks got to be part of that. Maybe get people's attention a little bit more. We can push this thing down to really low levels, if we'll just do the simple, easy things. We know that works.
How much stock can we put in these numbers? Testing is on a downward decline, and Mississippi maintains the highest test-positivity rate in the country. Are these numbers reflective of successful containment, or is there an artificial slump from a decreased rate of testing?
The rate of testing reflects the rate of illness. So like we saw before in May, and as we're seeing now, the demand is down because less people are more symptomatic. In Mississippi, we're not a wellness culture. We're an illness culture. We only get medical care if we’re sick.
So I think it is an accurate reflection of a decreased number of sick folks. And that's also reflected in other lines of evidence. We have had some leveling of new hospitalizations. I'll call doctors and say, “Hey, what are you seeing in your clinic? What is your experience?” and that is probably the most timely indicator. And they're just not seeing as many sick folks.
I wanted to talk about the death rate. We're in a tragic period for Mississippi. This is the unavoidable coda to the spread (in July). We're having death reports close to 50 for days at a time. Beyond those numbers, the hospitalization rate is stable. And those two things conflict in my mind. That tells me that the state’s hospital beds are being rapidly replenished as they're being emptied by death. Is that stable hospitalization rate masked by a sustained death toll?
Q&A with Dr. Thomas Dobbs on Racial Inequity of COVID-19 in Mississippi
State Health Officer Dr. Thomas Dobbs spoke with the Jackson Free Press in a phone interview on April 22, discussing at length the racial health disparities the COVID-19 crisis exposes. He described the steps the Mississippi State Department of Health is taking to address them in the future.
No, there's another measure we use—new daily hospitalizations, and that has declined and stabilized. So that's a better indicator for us that we're admitting less folks, but as you can imagine, there's a time course of illness, right? So someone gets sick, and usually it's (around) a week to 10 days or so before they go to the hospital, on the natural history of this illness. And then from that point, there's a time progression from getting sick to when they get better.
If they're hospitalized or they get worse, if they have to go to intensive care, there's usually a time period of supportive care and treatment where they either get better or they die. And that can take a long time. That can take four, five, six weeks.
So a lot of the deaths sometimes represent the cases that happened a month ago. And it's really a lagging indicator, as we've discussed, because it takes a long time for someone to get exposed, and then to get sick and die, on average. And so that's why we see this sort of strange undulation of cases.
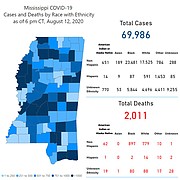
If you look at our mortality, you see that mortality slumped while we were having our youth outbreak, but then it popped up pretty remarkably as we go later into July and August.
What is keeping that hospitalization number so stable, if not new admissions on a higher rate than we're used to?
Well, it is new admissions. It's just moderated—it's not growing. It's always stacking on top of itself because there's so many cases in there, they take so long to go to the hospital.
We do have another measure where we look at new daily hospitalizations. Totally different measure than you've seen, probably.
Is that available on the website?
I have posted it before, but I don't think we have it on our website. Let me see if I can find it real quick, just for your knowledge. I'll send it to you.
We have about a thousand people at the hospital. So 45 deaths out of a thousand is really a small proportion. So if you look at our hospitalizations, we have 972 total hospitalized. And what you'll see is that total hospitalization number being stable, but the proportion of ICU patients increasing.
And the proportion of ventilated patients has increased, as you would imagine. But if you look at our new COVID-confirmed admissions, going back through May, the peak that we saw was later in July, at 137 admissions per day. And now we're at 105 new admissions—that was actually from yesterday.
That leads to another thing that I spoke to Dr. Woodward about at the end of last week. There is this problem of the long-haul coronavirus patient. These are long, long times to be spent in the hospital. To the degree that the next spike that we might see, we could have a huge portion of these people still taking up hospital beds. Can you speak to that in terms of our flexibility?
You’re exactly right. We are full to the brim and don't need to pour any more patients into the mix. She's exactly right. I agree with her 100%.
You're saying that testing follows illness—so if there is a decreased rate of testing, then that does indicate to MSDH that there is a decreased rate of exposure, and thus illness. But the Harvard Global Health Institute puts us at about 17% of our testing target. That is the second worst in the nation. Our test-positivity rate is the worst in the nation—20%. And that's four times what the World Health Organization suggests represents relatively controlled spread. Do you feel confident that our testing regime is keeping pace with the spread?
That's a dog-chasing-its-tail sort of thing. Because as your testing (positivity) percentage goes up, they recommend you test more people. I’ll tell you, Nick, we’ve approached this thing in such a piecemeal fashion. Instead of having a complicated equation, we've tried to break it down into simple arithmetic.
It's not the testing solution. It's not the social-distancing solution. It's not the medical solution. It's not the mask solution. These all interplay in a really big way. And if we have absolutely widespread community-based transmission, none of the other stuff matters. Not significantly.
So the contact tracing—that’s one of the other pieces. No individual one of these things needs to be fixed. They all have to be fixed in concert so that they come into proper alignment. We need to have adequate testing so that we can do surveillance and so that anyone who's sick or exposed can get tested.
We need to have the proper social-distancing and mask operations in place so that people don't transmit it but at a low rate. We need to have robust case investigation and contact tracing that can keep up with that. When all of those things are humming together in line, that's the response.
It's really artificial to look at any one of these things individually, and say you need to do this, or you need to do that. They all have to happen together. But if you have unmitigated community-based transmission, if you don't keep people from spreading it to each other by these sort of broad-based interventions, like distancing and delaying school, and all that kind of stuff, then you're not going to be able to catch up with the other things. There's no amount of testing that’s going to get you out of it, to be quite honest.
To the best of your knowledge, what is the current spread of coronavirus in the state’s schools? Beyond infections, how many students, across how many institutions, are currently quarantined?
I don't have an update from today, but I did (Tuesday). We had 29 schools—almost 30 schools, and 40-something people with coronavirus, with hundreds of folks being quarantined. We are working with the schools. They are supposed to submit weekly summary data to us from every school system. That would include information on the number of cases and the number of people quarantined by grade, that sort of information.
So that's something that we will make available to you. Right now we have piecemeal information, but you're seeing it, I know, in the news and social media. We know what's going on Corinth or what's going on in Gulfport, where they’re having a lot of kids out in quarantine. So that's going to be our big challenge.
And it is absolutely … not even remotely surprising to anyone who's been paying attention, and I know you have been. Because we've been saying for weeks, it's a hard time to open school. Even if you have no transmission in school, they would have so many kids showing up with it that you would have to quarantine a big proportion of every class that kid’s in. Week one in Corinth, in Alcorn County, which is sort of a low-(spread) county anyway, they had eight kids who walked through the door with it. They didn’t catch it there, but they walked into the school with it, and they had to quarantine like 150 people. So it’s really hard to operate school in the context of broad-based community transmission.
We've learned a few things about school outbreaks. First, schools don't have to publicly report when there's been an outbreak. Second, parents don't have to get their quarantined children tested. Third, school districts that we've examined generally have a positive test number—a percentage of students that triggers a broader shutdown. Finally, we know that middle-to-high-school age children are just as virulent as other carriers, but are more likely to have asymptomatic and lowly symptomatic cases. Putting all of this information together, we see the potential for Mississippi schools to be massive generators of asymptomatic, undetected community and familial spread of the virus: the engine of COVID-19 spread into the flu season. Is that a rational concern?
It's a very rational concern. You hit on the big points that really worry us—but the key mitigating strategy is if the schools are conscientious, if they vigorously embrace … (pause)
I mean, we felt more comfortable, we advocated for, we recommended virtual learning for the time being—not starting school right now.
But if the school is going to go to in-person learning, there are things that are useful. Number one, offering virtual (options), and trying to make sure that you depopulate the class for those who don't want to come in-person anyway; mixing virtual with traditional so that you can have less kids in the classroom.
The less kids you have in the classroom, it’s better spaced. Your transmission risks are going to drop dramatically. Mandatory masks are going to help, (having proper) airflow, not doing high-risk things where kids are all clustered together. Keeping them from being too close to one another for a duration.
If we can do these sorts of things, basically go into the school day assuming that every kid has coronavirus—if you go in with that mindset and plan it that way, you can really minimize transmission, but that's a big if. I think some of the school districts take it extremely seriously, and some are so annoyed with coronavirus that they want to ignore it.
But we know what happened with that in the summer. That's where our state’s collective consciousness was, to be tired of coronavirus. So we ended up spreading it around. And a lot of people died.
We've been talking to teachers from all around the state: hearing their experiences, seeing pictures and video. We’ve had teachers tell us that they have 20-plus kids in their class(es), so six feet of separation is physically impossible. So then, what they're being told in a lot of these districts is that 3.5 feet is enough. We’re seeing pictures of very, very large groups of student gatherings, often unmasked. Are the guidelines realistic based on what we're seeing so far?
I think what you're asking me is, are people following the guidelines? That's really going to be the rub. Those things are absolutely bad. And when we have kids who can't space properly, then a lot of those classes are going to end up being quarantined.
And that's what we're seeing. If we're going to do things that don't need to be happening—extracurriculars, nonacademic classes that could be put off and delayed—then we're going to have these things. We have a very clear set of recommendations that are aligned with those simple principles.
We're going to have trouble. There's no doubt about it. We're going to have a lot of difficulty. Some schools are going to do better than others. Some communities are gonna do better than others. It's going to be a tough fall. It's hard to imagine (not having) a tough fall. We're encouraged to have a little bit of a breather, of moderation in our daily reports. But we are not anywhere near a place where we can expect to have in-person school and not have a lot of people walking around with coronavirus.
State Health Officer Warns in Interview: Prepare For Overwhelmed Hospitals by Fall
State Health Officer Dr. Thomas Dobbs warns that there is no avoiding a catastrophic fall surge of COVID-19 hospitalizations, and is telling Mississippians to prepare for a season without access to emergency care.
You told me in our last interview that there had been no real disagreements between you and the governor. Reopening schools now represents the first time that the state has broken with the advice of you, MSDH, LouAnn Woodward and the urgings of medical associations across the state. Can you walk us through what led to this difference of opinion and difference of strategy?
I will say that, throughout our recommendations, even our recommendation to delay in-person school, we shared that and discussed it openly with the governor and his staff—to make sure they understood our perspective. And they respected that.
There is this, to me, a rather strange concept of ultimate district autonomy that seems to drive a lot of the decision-making process from Jackson. And so we felt strongly that we should make recommendations that schools delay opening. The governor’s staff felt very comfortable that we should be able to (publicly recommend delays).
So we have tried to promote delaying school. We've tried to promote a better mix of virtual and in-person learning. We’ve certainly tried to promote delaying extracurriculars. So we're going to continue to push for that, without a doubt. It's a tough balance, and we certainly understand that.
I will say that I want everybody to wear a mask. I think that's pretty obvious. But I do think that the governor's strategy of targeted and then statewide (mask orders) may have had merit. I do notice that places that are traditionally resistant to masks are actually using them now.
Do I wish people had been wearing (masks) all summer? Amen, I do—and doing the other stuff. But the psychology and the politics behind all of this is very delicate. It's easy for me to make pronouncements from a health perspective. That's actually pretty easy. It's the other part—it’s the mass psychology, and … frankly, sometimes it's the politics that gets in the way of good public-health action.
I understand we tread close—or into—the political and the ideological when we talk about this. But you mentioned this “strange ultimate district autonomy”—that’s something we’ve certainly questioned in the past month or so. Can you approach a pandemic with a hundred different strategies?
I think we'd be in better shape if we had a unified national strategy, and then a unified state strategy. But those are political questions.
I suppose, as a state and as a nation, we've accepted the downside of a lack of coordinated response in the interest of local autonomy. But that's a real political-science conversation, I'm afraid.
There's a lot of conversation about the challenge that virtual schooling poses to educational attainment. It’s broadly agreed that in-person learning is better than virtual learning. Would you also agree that in-person learning, interrupted by quarantine, which then becomes less-prepared virtual learning, is the worst thing that can possibly happen in terms of educational attainment?
I'll have to confess I'm not really qualified to give better pronouncements on virtual versus in-person. I can tell you my personal experience with my own child, who has done quite well with virtual, but his school embraces it aggressively.
And so it would seem that we have an equity issue in parts of education, where all kids need to have access to the same opportunities. That has stood out to me: This is a good opportunity for us to look at inequity as far as, (for example), broadband access, even if you're not in a coronavirus pandemic. One of my child's friends has to come over to our house and use the Wi-Fi to do homework. These are equity issues that transcend coronavirus, so maybe this is a good chance for us to address it.
Because of the challenges of switching back and forth between in-person and virtual classes, would a better strategy be quarantine-based? Where, once it hits a majority of students in quarantine, a school transitions to all-virtual, because that's the path it’s on at that point?
I'm not certain about the cutoff point, but every school needs to be prepared, because there's a good chance every single school might have to go to virtual, or distance learning. We're seeing a lot of it.
We do have some guidelines about when you consider closing school altogether, and what we shared with all the school districts is, if you have over three or more simultaneous clusters or cases within your school: multiple classes with multiple cases, y'all need to talk about closing school down for a couple of weeks and letting it cool down.
So, there are going to be instances where schools are almost certainly going to close, and it might be sooner rather than later. We do need to be prepared for virtual learning, because it's going to be a necessary reality for a lot of our schools.
If a school cannot manage the six feet of separation, if it cannot reach the basic guidelines, can that be mitigated or is it just not safe?
So, certainly, in a lot of our conversations, we understood the lack of perfection that can be achieved in a lot of locations. Kind of like our COVID response, our school response needs to be multi-layered.
But there are other things besides just the space—there are control issues that need to be considered. We really strongly recommend, if you have a class and everybody can’t be six feet apart, we strongly recommend cohorting the kids in age groups, so they're all in the same group and you don't cross-contaminate different groups, and they have strict seating locations.
COVID-19 Information Mississippians Need
Read breaking coverage of COVID-19 in Mississippi, plus safety tips, cancellations, more in the JFP's archive.
So if you have two kids that are 3 feet apart or 3-and-a-half feet apart, those kids are going to be within that zone of concern, but the kids in the next row are not going to be—the kids in the rows behind are not going to be.
And then also knowing that information you can identify who really needs to be quarantined in the event that you do have transmission. So there's a lot of layers of things to do. Certainly educating our kids is one of our priorities as a society.
It's a tough balance, and we'll try to give the kids, the students, and the teachers the tools they need, but it is a multi-factor approach, and we'll just have to try to deploy every tool. The main thing that would help is if there were less people in the community who had it, and where people were getting it. ... All of these people who came to school (with the virus) got it by doing stuff that they didn't have to do.
It was church trips, sleepovers, social events and birthday parties, things that no one has to do. But because we're just too darn impatient, we'd rather take the risk and get coronavirus.
We have to be more serious about this.
We need to have boring social lives for the next few months. Don't go to dinner with your friends. Don't have a birthday party. Don't have a wedding shower. Be boring for a while, exercise outside and get a little alone time, and that will make all the difference in the world.
State intern Julian Mills contributed to this report. Read the JFP’s coverage of COVID-19 at jacksonfreepress.com/covid19. Get more details on preventive measures here. Email state reporter Nick Judin at [email protected] and follow him on Twitter @nickjudin.
More like this story
More stories by this author
- Vaccinations Underway As State Grapples With Logistics
- Mississippi Begins Vaccination of 75+ Population, Peaks With 3,255 New Cases of COVID-19
- Parole Reform, Pay Raises and COVID-19: 2021 Legislative Preview
- Last Week’s Record COVID-19 Admissions Challenging Mississippi Hospitals
- Lt. Gov. Hosemann Addresses Budget Cuts, Teacher Pay, and Patriotic Education