Dr. Eric Topol, director of the Scripps Research Translational Institute, and nationally recognized expert on COVID-19, spoke to the Mississippi Free Press on the evolving threat of the delta variant, political resistance to pandemic containment measures, and the future of the virus. Photo by Michael Balderas
For much of the COVID-19 pandemic, Dr. Eric Topol, founder and director of the Scripps Research Translational Institute in La Jolla, CA has been a leading voice for a unified, swift response to the virus. Topol, a member of the National Academy of Medicine, and one of the most heavily cited living medical researchers, has informed public opinion on pandemic topics including the possibility for asymptomatic transmission of the virus, the nature of the delta variant and the potential fitness of variants still to come.
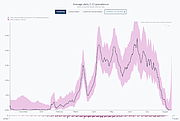
In late August, with the virus reaching its newest peak in Mississippi, Topol identified the Magnolia State as the global hotspot of COVID-19, reflecting the rampaging spread of the virus. That same day, Topol joined the Mississippi Free Press for an interview on the state of the pandemic—and what comes next.
Nick Judin: You noted that Mississippi in the last week has been the global hotspot for COVID-19. How can we appraise the specific cause of the upswing facing Mississippi today? Is it the climate pushing people inside? Low vaccination rates? The infectiousness of delta itself?
Eric Topol: Well, Nick, you touch on the key points right there.
Certainly, delta is ferocious. The most formidable variant of the virus we’ve seen so far. But this was exacerbated by the low rate of vaccination so far. Even if you’re fully vaccinated, you need to have a mask on—a high-quality mask, tightly fitted. You need to be distancing and staying outdoors as much as possible when you’re meeting people. You need to be maintaining ventilation when you’re indoors.
You need all these things, and they have to be practiced at the highest level. Really, what you need is leadership. You need the public-health officials in sync with the government. It doesn’t look like you have that there in Mississippi.
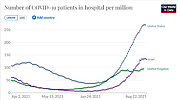
So far in this spike we don’t see signs of a downturn. How does India and the UK’s experience inform our understanding of delta’s future here?
That’s a good question. We don’t fully understand how India got turned around, with a lower vaccination rate—a considerably lower rate—than what’s in Mississippi or in Louisiana or Alabama. It appears that the virus burned through (the country,) efficiently finding hosts.
We know it moves faster and more efficiently than other viruses as well. So what appears to be the case? It burns through, and then as soon as it can’t find hosts, its descent can be as quick as its ascent, in terms of the number of cases that it generates.
Now, what’s interesting is that it isn’t stable. India is starting to trend up, the UK is starting to—more gently, but ascending. And that’s the trouble here. There’s still more people even after it does a U-turn and comes down. There’s still more people that are not vaccinated or have had prior COVID. It doesn’t mean that it’s permanently going to go away.
It has made a pass, and it could come back. And of course, it could come back in an even worse form—a worse variant.
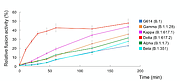
Everyone understands by now that delta infects more quickly and transmits much more rapidly. A lot of this has led to understandable fear over future variants. Are there other existing variants that we should be watching? And in general, what makes a variant concerning?
Right now, anything that can compete with delta would be very concerning.
Because this is so potent and so transmissible, and it even has some immune evasive properties. So there’s nothing right now that we’re seeing that effectively is competing with delta. Lambda certainly couldn’t do it.
One of the possibilities is that delta will acquire some additional mutations. And in fact, if you don’t sequence it, you could be missing that: delta, you know, with some added badness. Delta plus was put out there, which may be the kind of thing we’re talking about, but so far we don’t know of any changes in delta that are making it much worse.
But while right now there isn’t anything, that doesn’t mean that next week we won’t see something. That’s why genomic surveillance is so important. You’re not just looking for a virus that can stand up to delta at this point. You want to understand what it is about these mutations that makes it compete. That’s the secret: Why is it causing trouble?
With delta, we learned that it took a detour in its mutations. They’re very different from alpha, beta and gamma. We have to look for—not only the mutations, but why these mutations are selected for? Why are they doing so much damage to people?
I’ve had medical providers in Mississippi reach out to me and say that they are worried about delta plus. What about delta is deadly? What about delta plus is more so?
Well, we don’t need to make delta worse than it is. It is atrocious because of its (transmissibility). That’s why there’s more people in the hospital, more people dying.
We don’t have to assign it any more lethality. And we don’t have any definitive evidence that it’s (deadlier). We have one lab study that suggests some of the additive mutations of this so-called delta plus could make it a little bit more immune evasive. That is, for people who’ve had prior COVID, they’d be more susceptible to a reinfection.
Potentially, the virus may have a work-around to our vaccine immune response. But that is just tentative. We don’t have (the evidence) to be certain of that. It doesn’t mean that delta can’t evolve further and develop features like that.
I was watching a television program—Stephen Colbert—where my colleague, who I know well, Dr. Jon LaPook was saying ‘it’s more deadly.’ Well, no, it isn’t. We don’t have any data to (determine) that. I talked to him in advance of his appearance to try to give him information, but I guess I didn’t get him straight on that one.
When I speak to health-care workers across Mississippi, I’m hearing worse experiences even with much younger patients, compared to earlier variants. These are anecdotal—not research data—but how can we make sense of them?
Well, what you’re bringing up is very tricky to try to ferret out. The fact is, when it’s spreading so much, and you’re shielding the older people who did get vaccinated, you’re naturally going to see attacks in younger people.
But is the virus per se leading to worse disease? It’s possible, but we haven’t nailed that down.
What we do know is that the viral load is over a thousand times higher. That in itself would of course be worrisome—that it could overwhelm a person when you have that much viral inoculation. So it’s possible, Nick, but it’s still (indeterminate).
What does the future of COVID-19 look like? Does it become endemic? Does it reach what we might call peak fitness, beyond which explosive new variants are less likely to emerge?
It’s hard to say. It’s possible that we have reached peak fitness. That’s the optimistic view. That’s what I’ve written about with my colleague, Dr. Roberto Burioni. I think the unknown is could we get something worse than delta? I sure hope not. This thing is a freaking monster. We don’t need to go there.
On the other hand, the United States is now the number-one producer of COVID infections in the world. We are a petri dish to cultivate new variants here. It will take a lot to override delta. Delta is taking over the whole world. Every country in the world is going to be delta-fied, if you will. It’s just a matter of time. Most of them already are.
So while we may not get something that’s worse, there are some evolutionary virologists saying that the sky’s the limit. It could get even worse and potentially could fully evade our vaccines. It has already punched some holes in our vaccine, but it’s possible that we’ll see another version of the virus with another Greek letter that could prove much more vaccine-resistant. But so far they’ve held up.
And that’s what is so striking. I wrote just this morning, asking “how can we have vaccines that are leaky for infections, but hold up so well for hospitalizations and deaths?” The answer, to simplify, is that it’s leaky because of (declining) neutralizing antibodies. And that’s what boosters get back up to high levels.
But the pneumonia from COVID and all the other organ damage are mediated more through T-cells, which are present after vaccination. So that’s why we’re having this split. The vaccines are leaky (for infections). They’re not doing as well, more at the 50% level even where they used to be at 90% plus protection.
That’s bad. We don’t want infections. You yourself know very well what can happen when we see lots of infections. A portion of those will go on to become hospitalizations. Some of those will go on to deaths, (even) in vaccinated people.
So the number-one thing we’re not doing is blocking cases—blocking new infections. And we’re impaired now because our vaccines are not working as well. We do not want to get something worse than this. But fortunately, thank goodness, for the most part they’re holding up pretty well (with) just a few percent of a slide so far, with respect to hospitalizations.
Can you speak a little bit more about the short-term and the long-term immune responses?
When you get the two shots—particularly the second shot, where delta is concerned, a couple of weeks later you’ve got a really good T-cell response, the so-called CD4/CD8, which are basically on demand. They’re the military reserve, and they’re called up when you have an infection.
(These cells) are doing their job after the vaccine. Whether it’s Pfizer or Moderna, they’re doing their job and doing it pretty well. Not perfectly, and not as well as before delta.
But the real problem is blocking the infection. What we’d really like is called mucosal immunity. Perhaps where you took an intranasal vaccine, and now you’ve got something called IgA antibodies in your nasal mucosa and your upper airway.
And so here you never let COVID get into your body at all. You never let this virus get into your upper airway, which is the port of entry for almost everyone. Rarely, it can get in through your eyes or some other pathway, but it’s almost always the nose or the mouth, the throat.
I wish we had a nasal vaccine. I wish we did. That would be very popular. Get it, mail it to people, and they could just take an inhalation and be good to go. No needles! We would love that, and we need it now, but it only exists in early trials.
So what the shots do, rather than the nasal vaccine, is produce these neutralizing antibodies. This is another way of blocking the entry of the virus into our cells. Now, at first they did that really well. The neutralizing antibodies in our blood—called IgG antibodies—did that great until delta came along. Now they’re just not holding up that defense.
It’s like our football team that lost half its line. The virus is just penetrating and running through it. It’s still holding up to some degree, but only at about half of what it was. That’s our problem right now. We are on the defensive. We have the T-cell reserves to block the pneumonia and everything else that this virus can cause, but (for transmission) we’re not bringing in the other tools in our kit: masking, distancing and ventilation, all of these other tools.
We’re just not (using these tools). I’m in California. Actually, I was in the clinic today, and I have to say, it was great. My patients were so diligent. They are coming in wearing n95 masks, better masks than some of the doctors and nurses. That was pretty cool because we’re indoors, we have no ventilation, we’re in a small clinic room.
But if you walk around, there’s not a lot of people here observing any of the guidance. And if they do, it’s over their chin or under their nose, and it’s cotton. This is what we’re dealing with. It’s not just stupidity. It’s a lot of people that just don’t want to be part of this whole pandemic, unfortunately.
And the government should have made it a priority to distribute high-quality masks. They could’ve gotten them for 50 cents: kn95s sent to every household, enough for every American. It’d be cheaper, they could’ve had “USA” or “Mississippi” on it. But we didn’t do it.
Mississippi just got a new flag.
Yeah! Put the flag on there. Make people proud of wearing a mask. It’s really important as an additive feature.
Our governor has been very resistant against the concept of masking. His explanation to us most recently was that telling folks to mask after vaccination harms the vaccination effort. What do you make of the masking question?
Well, up until delta, in April and May, we were good without masks. The vaccine was so effective that the masks weren’t as necessary.
It’s really when delta comes on board that you could end up in a room with unvaccinated folks who could potentially infect a vaccinated person. And this is when vaccination and masks come into play. The notion that vaccines were going to carry us was fine until we got this really vexing variant. This virus is so infectious. That’s the problem. The vaccines are leaking, and you patch up the leak with a mask. If it’s worn right, it covers your face, and it’s high quality, well, even better.
To people saying “if you still need a mask, the vaccines don’t work,” that is idiotic. That’s misinformation. It’s just not right. The problem we have, Nick, is the circulation of so much misinformation that it indoctrinates people. They don’t know any better because it’s been inculcated in their minds, unfortunately.
Here in Mississippi, after reporting the tragic death of MKayla Robinson, we immediately started receiving disgusting comments assuming things about her health, weight, pre-existing conditions. Misinformation wasn’t from any one source; people came up with it themselves.
We’re facing so many fabrications. So many distortions. Folks are just making stuff up. I think this escalated during the Trump years; he would make stuff up and this process has become rampant. We have people saying, if you get vaccinated, you become sterile. That there’s microchips in the vaccine.
We have your case: people making stuff up about a horrific case of a young girl who died from COVID. People are getting away with lies like never before. Separating truth and fact from all that is what your whole mission’s about. And I know it’s become harder because of all these fabricators, these liars.
I think when, for four years, the president is lying every day—multiple times a day—it gives license to anyone. And that’s unfortunate. Obviously it doesn’t mean we didn’t see this occurring before then, but not this sea of misinformation … these overt lies.
I mean, there is some kind of nonsense about it integrating with your genome, people calling it experimental gene therapy, all this total bullshit! The folks making this up are predating on people who don’t know any better.
And it’s really sad. I’ve never seen this before. I’m an old dog, and I’ve never seen it to this degree. We just don’t need it. Look at the countries who’ve done really well. They stick together. They stick to the facts. They know they have a common enemy. They don’t make all this stuff up like here.
Let’s shift gears to booster shots, which are on everyone’s mind. What’s the importance of the booster shot?
Boosters are going to be very important. At first, I was very much against them. Because it was coming out of Pfizer and then Moderna, and it was on limited data. Talk about a conflict of interest, right? Obviously, they’re going to be advocating boosters. I bristled then, because we can’t even get people the first shot; how are we going to get third shots in?
But you know what happened next. When I put out the fact that we had slipped down to 50% (efficacy at preventing symptomatic infection) for our vaccines—that they were leaking—it didn’t go over well on Twitter. I said I was estimating 50% to 60% efficacy, and I was being optimistic.
It could be down below 50%. People are in denial, just like when Israel came out with their numbers saying 40% reduction in efficacy, (folks) were taking it apart, making stuff up, saying the Israelis don’t know how to analyze their data. Wrong, wrong, wrong.
We do need boosters. We see now in Israel, which has got more than a million people on boosters, they just dropped booster availability down to age 40. They’ve got people over 60. They’re now working on over 50. They keep dropping it down. Most of their population will have boosters soon. I don’t know if we need them all the way down to age 40, but certainly in the higher age groups.
The point is, if your vaccine efficacy is dropping down against infections towards 50% or 40%, that’s really weak.
Do you want to go on an airplane? With all these other people in this country that don’t even have to be vaccinated. Do you want to go on a train or a bus? You want to take an Uber ride? I mean, what do you want to do when you’re that unprotected? So if you basically want to live again with your vaccine working like it’s supposed to, there’s your booster shot, right?
The good thing for us is that we’re lucky to be in a country that can access these boosters. Most of the world doesn’t have access to these vaccines like we do. That’s absolutely unfair. We need to do both. We need to help all those places (with our supply). We need to be the real leader in the vaccine effort. Right now we’re trailing.
We’re not putting out the data. We have to watch Israel and the UK, watch what’s going on in the rest of the world. So even though we’re not the vaccine leader we should be, boosters are going to be important for us. And I hope that we can ramp up production and supply of the vaccine and do much better for the rest of the world.
Many people have asked me if booster doses should be mixed—different sources than the original dose.
Well, there’s one booster that looks like a winner. I mean, a real winner. The mix—the crossover (to mRNA) is better than the two shots themselves. We know that it’s the case. If you had AstraZeneca, which isn’t in this country, and then you had either Pfizer or Moderna, it’s just … wow, that immune response.
How does Johnson and Johnson compare?
I’m guessing it will be comparable, but we don’t have the data, yet. But I’d be very surprised if it isn’t. So I’d like to see all the people that got J&J to get an mRNA shot. Don’t get another J&J because it won’t be as effective. And you know, that it looks like it’s going to be one great solution, and frankly, should have happened by now.
We should have the data. Where is Johnson and Johnson? Where’s the data? If you extrapolate from AstraZeneca, you would conclude that if you go in the order, the best thing is, first, if you had prior COVID and you get at least one shot, that’s powerful. There’s nothing like a natural infection. But we don’t want people to have those natural infections. Still, if you get one, and then you get your shot, that is very immune.
The next is viral vector plus mRNA. Now, this is very important. It doesn’t work the other way around. if you’re starting with an mRNA, and then you get a J&J, it doesn’t look like there’s anything (good) there. So the order is important. Beyond that, it doesn’t really matter if you get, say, a Pfizer and then a Moderna.
We don’t have any data to suggest that makes a difference. I mean, Moderna looks slightly better than Pfizer right now, but that could be because the dose that they selected in their vaccines was relatively high. That’s why Moderna folks had more side effects. But they’re going to drop the dose down to half in the booster phase. So that may not be a lasting advantage.
Should people get the first booster available, or hold out for delta-specific boosters?
That’s an important question. It looks like the original vaccine booster is inducing such high neutralizing antibodies—and likely also priming memory B cells—that it will work quite well. We won’t be seeing a delta-specific vaccine for many months since that has to go through formal clinical trial testing for both safety and immune response. A delta-specific booster would be ideal, and even better, a pan-coronavirus vaccine as a booster, in the times ahead. But for now, the original should do the trick.
Is the pan-coronavirus vaccine something we hope to see soon?
If we put our foot on the accelerator and give it number-one priority, I do believe we could get it by 2022 sometime. Then we wouldn’t have to worry about each Greek letter variant. Since it is so multi-potent, it would be expected to have efficacy across all variants.
What’s our current understanding of long COVID?
Well, talk about lacking data. That’s another area where we (aren’t sure). There are people who got infected in March 2020 that are here, in August 2021, still hit with symptoms that are very disabling. It’s variable. Some people, after a few months, are returning back to baseline. Some people have gone well over a year, and they still can’t walk around the block.
They have brain fog. They’re not functioning like they used to be. These can be young, healthy, athletic people. It’s just all over the place.
Do we see a reduction in occurrence, severity or length based on vaccination status or antibody treatment?
With long COVID, there was some hope that the vaccine, for those people, might rev up their immune system, but we just don’t have any good data. There’s just anecdotes. We don’t know.
If you had a breakthrough infection, it is possible you could get long COVID. That’s what early data from Israel looks like. We don’t (entirely) know. We’ll have to see about that.
As far as the monoclonal antibodies, that does inactivate the virus. If you use a cocktail of antibodies, the hope would be, if you get COVID and you get monoclonal antibodies, that this would reduce the chances for long COVID. But again, there’s just not the studies to back that up yet. Right now it’s still a theory.
Back to the subject of misinformation, we have a concerning number of Mississippians self-medicating with Ivermectin. Which of these alternative treatments are worth consideration?
None of them are worth considering, including ivermectin, which has got all sorts of warts. I mean, it’s possible ivermectin could have some results, but we have no data to prove it. And the biggest study had to be retracted because it had very serious flaws in the data. And it’s only considered in clinical trials right now.
Ivermectin is an anti-parasite drug. It’s used for … river blindness, you know? Things like that. We have no data to warrant people taking ivermectin, and there have been a lot of false claims out there about it.
The only thing we have that prevents COVID, that’s been proven, if you’ve had a known exposure, is to take an injection, under the skin, of monoclonal antibodies, which is now FDA cleared.
We have nothing else at this point. And then if you get sick and you’re in the hospital, then steroids can help—but we just don’t have much to work with there. That’s why prevention is the fundamental goal.
Delta is significantly more infectious. Help our readers understand what that means, practically.
I came up with this term to explain it: the delta stress test. Don’t give your vaccine the delta stress test. You don’t want to do that. Help your vaccine. Scaffold it with your mask, stay away from other people in enclosed spaces, stay away from indoor gatherings, depend on ventilation and filtration.
So that’s how I communicate. You had your vaccine. Don’t give it a stress test. We will get through delta. We will get over this hump in the weeks ahead. And (when that time comes), if you want to try to go without a mask indoors and what-not, that’s different, but not right now.
This is where we got into the jeopardy zone. Serious jeopardy.
Any parting words for Mississippi, Dr. Topol?
I’ve been in Mississippi. I have relatives in Mississippi. I’ve been to Jackson and Biloxi and many other parts of the state. I feel for the people there.
It’s horrible. Getting through this—the worst time in the pandemic, and now the worst state affected, it’s dreadful. Sadly, a lot of it was truly preventable, and it’s on the leadership there for not having conveyed things better, not having better communication.
It’s not just here. A lot of states that are similar to Mississippi are also affected very similarly, including neighboring states. And you know, this (wave) started in Missouri and Arkansas. That should have been the 911 call. They should have gotten serious then, when we knew where it was headed.
We didn’t do the right thing. The saddest part about this is that it’s an avoidable tragedy. But it’s not too late to gear up. We’re not done with this pandemic, yet.
This interview is condensed and edited for clarity.
This story originally appeared in the Mississippi Free Press. The Mississippi Free Press is a statewide nonprofit news outlet that provides most of its stories free to other media outlets to republish. Write [email protected] for information.